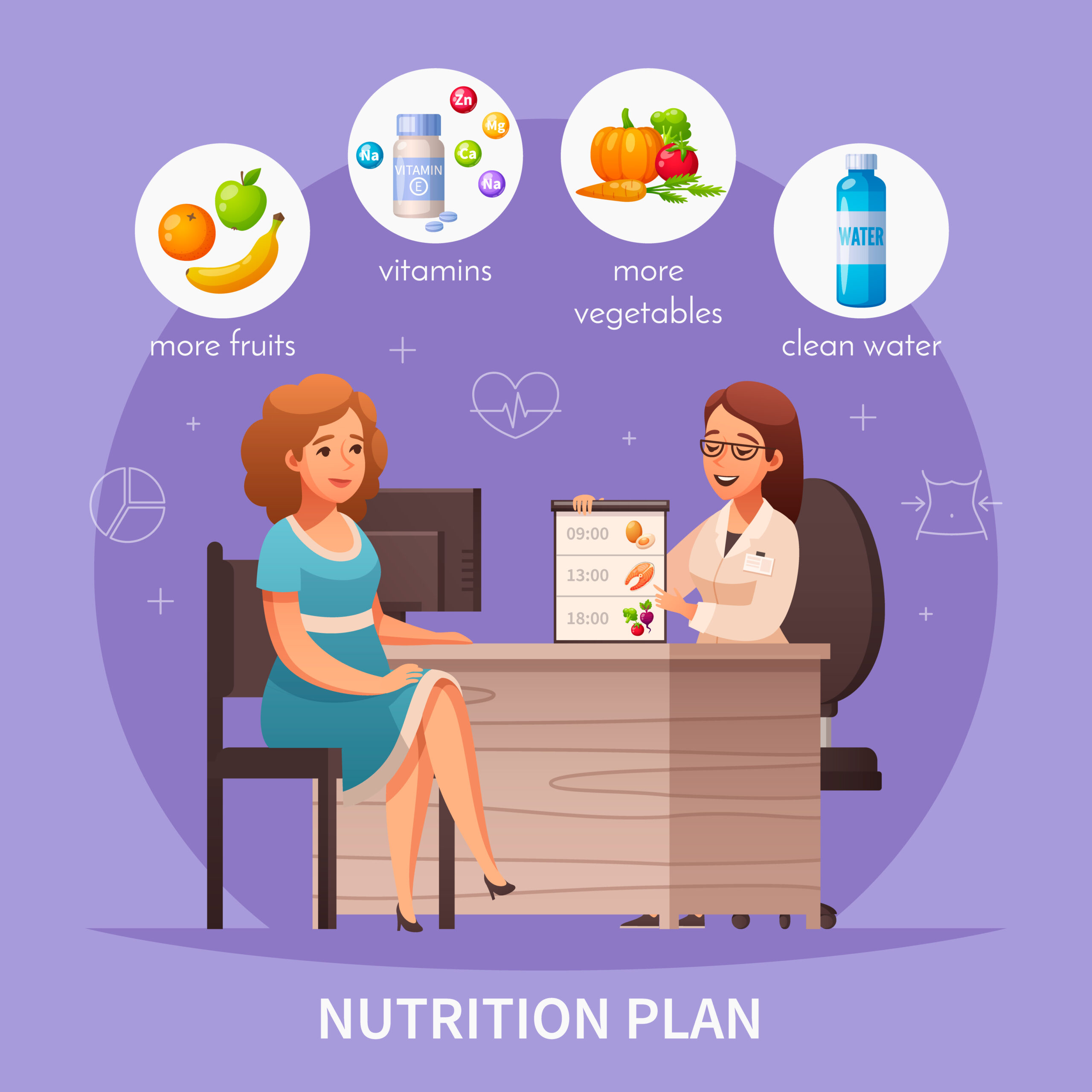
To support your body’s healing and milk supply after birth, focus on these nine essential nutrition strategies every day:
- Make protein a daily priority for strong postpartum healing.
- Focus on iron-rich foods and pair them with vitamin C for better absorption.
- Include healthy fats to stabilize hormones and support recovery.
- Stay well-hydrated to naturally protect and improve milk supply.
- Add calcium-rich foods like dairy, ragi, and sesame to protect bone health.
- Increase fiber gently to avoid constipation during recovery.
- Rely on small, frequent meals to maintain steady energy.
- Enjoy traditional postnatal foods as supportive extras.
- Avoid restricting food early on so your body and milk supply stay strong.
The Postnatal Nutrition Truth No One Talks About
Look, nobody tells you the real story about eating after delivery.
People expect you to recover right away. You need to feed the baby. You’re told to get some sleep — an idea that often feels laughable. At the same time, you must eat well and allow your body to heal. This recovery period is like running a marathon, and you have to do it all while surviving on almost no sleep.
From what I’ve seen while working with new moms at Advamed, one pattern shows up again and again — the postnatal diet is often treated as an afterthought. Everyone focuses on the baby, which makes sense. But here’s what actually happens: your body has just gone through massive physical stress. Whether you delivered naturally or had a C-section, you need serious nutritional support — not the generic “eat healthy” advice, but actual recovery fuel.
So let’s break down what works. Based on data, patient outcomes, and what we’ve tested with hundreds of mothers.
1. Protein Isn’t Optional, It’s Your Foundation
During the first 6 to 8 weeks after delivery, your body is repairing tissue at an accelerated rate. You need around 70 to 80 grams of protein daily — and that’s not a suggestion.
Here’s the kicker: most new moms we talk to are getting barely 40 grams. They’re surviving on whatever’s quick — biscuits, toast, maybe some dal. It’s simply not enough.
What actually works? Split your protein intake across meals. A paneer paratha at breakfast gives you 15–20g. Chicken or fish at lunch adds another 35g. An evening snack with yogurt and nuts contributes around 12g. You reach the target without overthinking it.
We tell moms at Advamed to think of protein like medicine. You wouldn’t skip antibiotics because you’re busy — the same logic applies here.
2. Iron Replenishment Takes Months (And Nobody Warns You)
Giving birth involves blood loss, which lowers your iron levels — and this is important to understand. It happens even when the delivery has no complications.
The extreme tiredness you feel is likely not just from lack of sleep. Low iron causes a very specific kind of exhaustion — a deep, full-body weariness that rest simply can’t fix.
Lab work shows that most postpartum women have ferritin levels below the optimal range for months. The body prioritizes iron for breast milk, which means you are last in line.
Spinach and dates help, but absorption matters more than intake. Pair iron-rich foods with vitamin C. That morning mosambi juice with your iron supplement? It’s actually strategic. Avoid tea right after iron-heavy meals, as it blocks absorption by 60–70%.
Here’s what I’ve seen working: slow-cooked meat dishes (if you eat non-veg), beetroot in salads, jaggery in moderation, and a good-quality supplement. Get your iron levels checked at 6 weeks postpartum. Don’t guess — just test.
3. Healthy Fats Are Non Negotiable for Hormones
Your body is recalibrating an entire hormonal system. Estrogen drops, prolactin rises, and thyroid function shifts. All of this requires fat — actual dietary fat — to function properly.
The funny part? We still see patients avoiding ghee and coconut oil because some article from 2010 said fat makes you fat. Meanwhile, their hair is falling out and their mood is crashing.
Omega-3s are especially important. They reduce postpartum inflammation and support brain function. Walnuts, flaxseeds, and fish are excellent sources of healthy fats. We recommend two to three servings of fatty fish per week, or a quality omega-3 supplement.
A tablespoon of ghee in your dal, coconut chutney with dosa, almonds as a snack — these are simple ways to meet your needs. You require roughly 30–35% of your daily calories from healthy fats during postpartum recovery. Advamed’s nutrition protocols reflect this. It’s evidence-based, not traditional wisdom dressed up as medicine.
4. Hydration Affects Milk Supply More Than Any Other Factor
Everyone talks about fenugreek and lactation cookies. But do you know what actually boosts milk production fastest? Hydration.
You’re losing fluid through nursing, night sweats (which nobody talks about enough), and general recovery. If you’re not consciously drinking water, you’re likely 500 to 700 ml short of what your body needs each day.
Aim for 3 to 4 liters. Sounds like a lot? Break it down: one glass every hour you’re awake. Coconut water counts. Soups count. Buttermilk absolutely counts — and it adds probiotics.
What I tell moms is simple: keep a water bottle within arm’s reach during every nursing session. You’ll finish it without even thinking about it — that’s 8 to 10 extra glasses right there.
5. Calcium Doesn’t Just Come From Dairy
Breastfeeding pulls 200 to 300 mg of calcium from your body every day. Your bones are literally donating minerals to support milk production. This isn’t a scare tactic — it’s physiology.
Most women focus only on dairy, which is helpful if you can tolerate it. But there are other excellent sources too: ragi, sesame seeds (til), amaranth, and fortified foods. Just one ragi malt in the evening can give you around 350 mg of calcium, plus iron.
We’ve seen bone density scans from women who didn’t prioritize calcium postpartum. The difference is measurable. Five years later, it shows up as early osteopenia — something that’s entirely preventable with consistent calcium intake during the first year.
Supplement if needed. Calcium citrate absorbs better than calcium carbonate, especially if you have digestive issues. And remember to take it separately from iron for optimal absorption.
6. Fiber Prevents the Constipation Nobody Wants to Discuss
C-section recovery combined with pain medications? You’re almost guaranteed to experience constipation. Even after a normal delivery with stitches, the concern is the same.
Straining is the last thing you need, yet I often see women cutting back on fiber-rich foods because they feel “too filling” or they assume these foods cause gas.
Here’s what actually helps: increase fiber gradually. Start with cooked vegetables, oats, and well-cooked lentils. Add raw vegetables and fruits as your digestion stabilizes. Papaya is especially helpful because it provides both digestive enzymes and fiber.
Prunes work — and no, they’re not just for elderly people. Three prunes before bed can regulate bowel movements within 24 to 48 hours. Adding ground flaxseed to your morning smoothie or yogurt is another simple fix. These small changes can prevent a very painful problem.
7. Small Frequent Meals Beat Three Large Ones
Your body is working overtime — digestion included. Large meals divert blood flow and energy to your gut at a time when you need that energy elsewhere, like producing milk or healing tissue.
Six smaller meals spread out nutrient delivery, keep blood sugar stable, and prevent the 4 p.m. crash that makes you reach for sugar.
Here’s what this looks like in practice: breakfast at 8 a.m., a mid-morning snack at 11 a.m., lunch at 1 p.m., an evening snack at 4 p.m., dinner at 7 p.m., and a bedtime snack at 10 p.m. Each should include protein, some healthy fat, and complex carbs.
The bedtime snack matters more than most people realize. Nursing overnight means your body needs fuel. A banana with almond butter or a small bowl of oats can support both milk supply and sleep quality.
8. Traditional Foods Work (When Science Backs Them)
Methi laddoos. Gond katira. Panjiri. I’m not going to dismiss these just because they’re traditional.
What I’ve learned from reviewing research is that many traditional postnatal foods do have legitimate nutritional benefits. Fenugreek contains compounds that may support lactation. Gond (edible gum) provides protein and minerals. Dry fruits and ghee offer concentrated calories and nutrients.
The problem arises when these foods replace balanced meals — or when someone with gestational diabetes eats six laddoos a day without monitoring blood sugar.
Use traditional foods as supplements to good nutrition, not replacements. That’s the balanced approach we take at Advamed Hospital: respect the wisdom, verify it with science, and adjust it for individual needs.
9. Don’t Restrict Calories While Establishing Milk Supply
This deserves its own section because I see it constantly — women trying to “lose baby weight” at just 3 to 4 weeks postpartum by cutting calories.
Your body needs 450 to 500 extra calories a day while breastfeeding, on top of your baseline needs. If you restrict too much, your milk supply drops, your energy crashes, and your recovery slows down.
There will be time for weight management. The first 8 to 12 weeks is not that time. Focus on nutrient density instead of calorie counting. For most women, weight naturally comes off between 6 to 12 months postpartum when they’re eating well and moving normally.
What matters right now: recovery, milk production, mental health, and rebuilding your energy reserves — not fitting into pre-pregnancy jeans by some arbitrary deadline.
Here’s What Actually Matters
New-mom nutrition isn’t complicated, but it is specific. Your body has essential needs during postpartum recovery, and meeting those needs isn’t indulgent — it’s basic maintenance.
At Advamed, we work with each mother individually because what works can vary widely. Some need more iron support. Others require thyroid monitoring. Some develop new food sensitivities during pregnancy.
But the foundations stay consistent: adequate protein, replenished minerals, healthy fats, proper hydration, and enough calories to support healing and lactation.
You just did something physically extraordinary. Feed yourself accordingly.
If you need personalized guidance on your postnatal diet, we’re here to help — with real assessments, practical plans, and support that goes beyond generic advice. Because recovery matters just as much as delivery.
FAQs
Protein-rich foods like eggs, chicken, lentils, and dairy are the best for healing. Pair them with iron sources (spinach, dates), healthy fats (ghee, nuts), and plenty of water to support energy, hormones, and breast milk.
We give you a simple, personal food plan that helps your body heal and keeps your milk supply strong. We focus on the most important foods like protein, iron, and water and show you easy ways to eat well every day.
Common issues include low energy from low iron, constipation from reduced fiber, hormonal mood swings, dehydration affecting milk supply, and bone weakness from calcium loss. Eating the right foods can help prevent and ease these problems.
Focus on daily protein, iron with vitamin C, healthy fats, and enough water. Eat small, frequent meals to keep energy steady, include calcium-rich foods, and avoid cutting calories too soon to support both healing and breastfeeding.
Yes. We use trusted traditional foods that help recovery, and combine them with proven science. This makes sure you get the right nutrition in a way that’s safe, healthy, and works for you and your baby.